Where Senses Meet
In the vast architecture of the human brain, it is easy to become transfixed by the grandeur of the cortex—the site of language, logic, memory, and conscious will. Yet before any of these functions can unfold, something more primal must occur: the integration of sensation. For the brain to think clearly, it must first feel clearly. And that process begins not in the heights of cognition, but in the depths of the brainstem.
Multisensory integration—the ability to combine sight, sound, motion, and touch into a coherent experience—is foundational. It is how a newborn orients to a voice, how a driver responds to a sudden movement in peripheral vision, how one navigates through space without conscious calculation. This process happens rapidly, often without awareness, and always before deliberation.
The brainstem, nestled just above the spinal cord, serves as the first meeting place for the senses. Within its compact structure, signals from the eyes, ears, skin, and muscles converge. Here, neurons do not wait for permission to act. They fire in response to the world, aligning gaze with sound, posture with motion, breath with emotion.
This article explores the role of the brainstem in multisensory integration—a role both ancient and essential. It examines how this region supports balance, orientation, and readiness; how it enables higher cognition by quietly stitching together the body’s streams of sensation; and how its dysfunction reverberates into every corner of experience. It also reflects on the therapeutic significance of beginning with the brainstem, particularly in interventions like Optometric Multisensory Training (OMST), where healing starts from the bottom up.
The Brainstem: Structure and Function in Sensory Processing
The Architecture of an Ancient Conductor
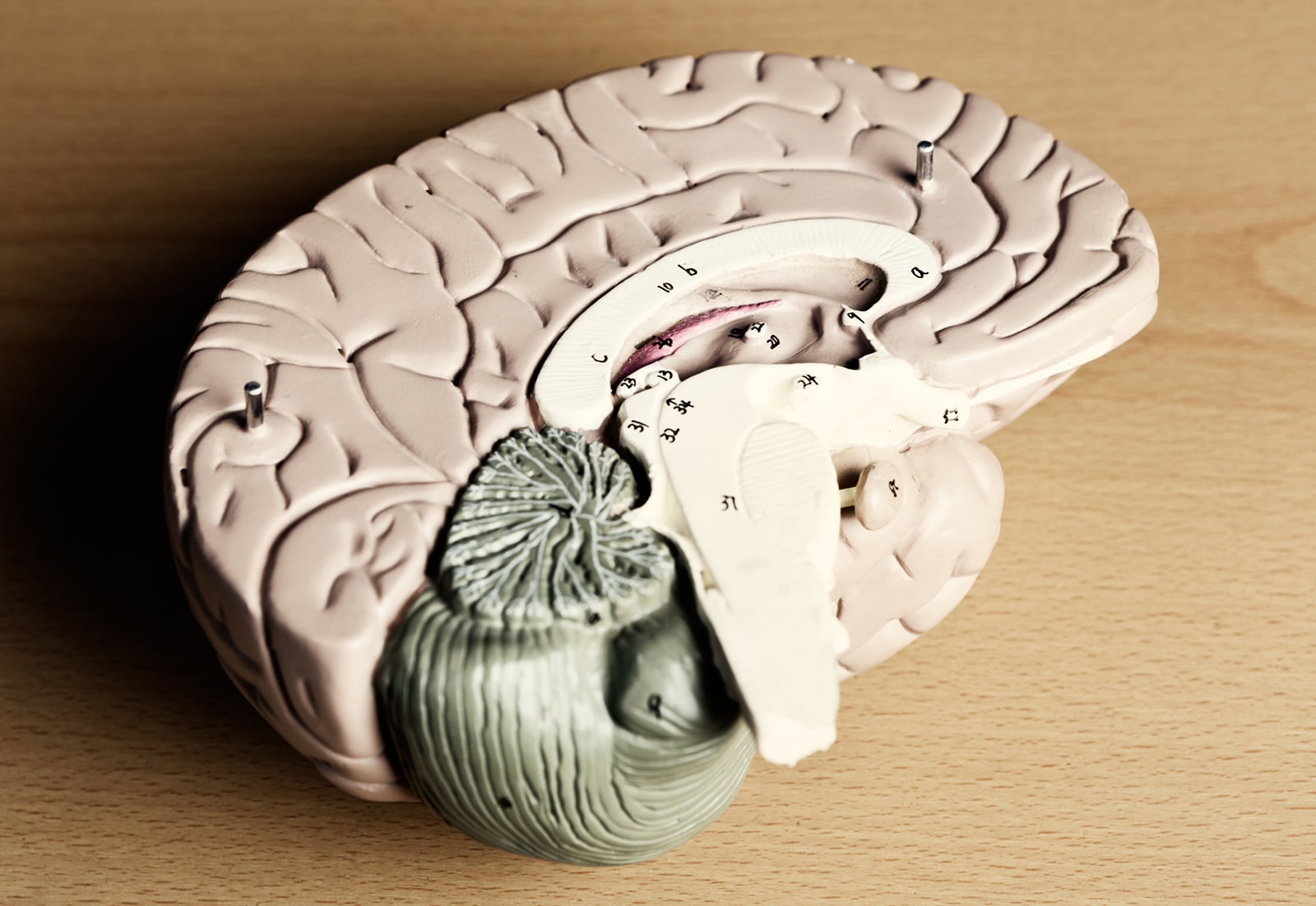
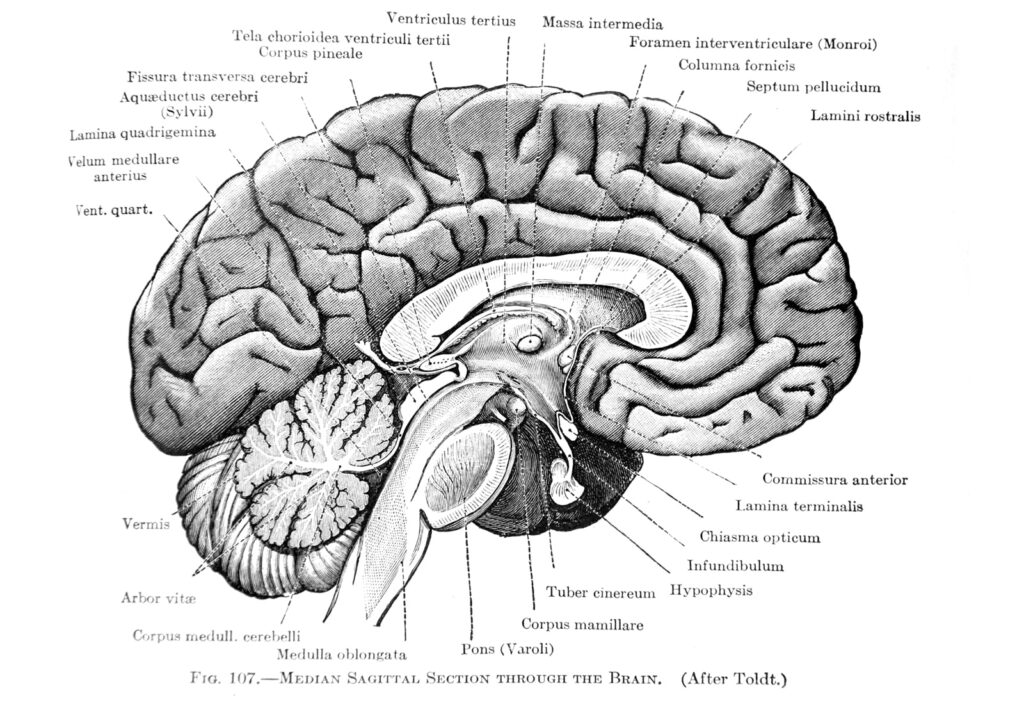
The brainstem, though small in size, holds immense power. Composed of three primary structures—the midbrain, pons, and medulla oblongata—it serves as both gateway and governor, channeling signals from the body into the brain, and from the brain back into the body. It is here that much of the sensory world is first registered, processed, and acted upon.
The midbrain, or mesencephalon, is perhaps most crucial in the context of multisensory integration. Within it lies the superior colliculus, a layered structure that receives input from the eyes, ears, and skin. Just below, the inferior colliculus processes auditory input. Together, these structures help the body orient toward relevant stimuli—a flash of motion, a sudden sound—long before conscious thought is engaged.
The pons and medulla contribute as well. The vestibular nuclei, housed within the pons, integrate signals from the inner ear’s semicircular canals to regulate balance, posture, and eye movements. The reticular formation, which spans both pons and medulla, modulates arousal and attention in response to incoming sensory data, preparing the cortex for what comes next.
The First Platform for Multisensory Processing
The brainstem is not merely a relay station. It is a processor in its own right—performing early-stage analysis of incoming signals. This includes aligning spatial information across sensory modalities, such as synchronizing what is seen with what is heard. This cross-modal alignment begins in the superior colliculus, where neurons respond most robustly when visual and auditory stimuli are temporally and spatially aligned.
This process serves vital functions. It allows for quick orientation toward danger or interest, calibrates eye and head movements, and helps maintain postural equilibrium. When a person hears a sound to their left and sees a movement in the same direction, the brainstem coordinates these clues into a unified perception of where to look or turn.
Such integration is foundational for navigating daily life. Without it, the world would be disjointed—sight delayed from sound, motion dislocated from space. The brainstem provides the thread that begins to weave the sensory world into a coherent tapestry.
Bidirectional Flow: Sensory Input and Motor Output
What enters the brainstem does not remain there. Once sensory information is processed and synthesized, it generates appropriate motor responses—some reflexive, others preparatory for higher-order action. Eye movements, head turns, balance corrections, and changes in muscle tone often originate in response to integrated sensory input within this region.
The vestibulo-ocular reflex (VOR) is one such example. It stabilizes vision during head movement by coordinating the activity of eye muscles with vestibular input from the inner ear. This reflex depends heavily on brainstem circuits, and its dysfunction is a hallmark of sensory disruption following concussion or vestibular disorder.
In this way, the brainstem is both receiver and responder. It governs a loop of input and output that operates beneath awareness but shapes every moment of interaction with the environment. From stepping off a curb to catching a ball, this loop makes seamless action possible.
A Foundation for Cortical Learning
Before higher cognition can occur—before attention can be focused, language acquired, or memory encoded—the brain must first make sense of the sensory world. The brainstem lays this groundwork. It is, in developmental terms, the first processor, enabling infants to begin orienting toward sound, tracking movement, and feeling touch.
When this foundation is solid, higher cognitive functions can build efficiently. When it is fragmented, those functions may never fully stabilize. Disruptions in brainstem-based processing are increasingly recognized in conditions such as autism spectrum disorder and ADHD, where sensory integration difficulties often precede and complicate cognitive and emotional regulation.
Therapies that address these early-stage processes—particularly multisensory therapies that stimulate and retrain subcortical systems—aim to restore a level of integrity to this foundation. In doing so, they may unlock potential in regions of the brain that cannot function well until the sensory groundwork is firmly in place.
Multisensory Neurons and Early Integration
The Superior Colliculus as Convergence Center
At the heart of early multisensory integration lies the superior colliculus, a structure perched atop the midbrain like a vigilant sentinel. Its job is to detect and align sensory events across modalities—especially those involving sight and sound. When a loud noise occurs to the left, and a flash of motion follows in the same direction, neurons within the superior colliculus fire not just in parallel, but in concert. This synchronization allows the brain to localize stimuli in space with remarkable efficiency.
The superior colliculus is organized in layers. The superficial layers primarily process visual input, while deeper layers receive and integrate auditory and somatosensory signals. Neurons in these deeper zones are multisensory by design—they fire more robustly when input from multiple senses converges. This property, known as superadditivity, allows for faster and stronger responses to complex environmental stimuli than to unisensory input alone.
In practical terms, this means the superior colliculus governs our instinct to turn our heads toward unexpected sights or sounds. It also plays a role in initiating saccadic eye movements—the rapid shifts in gaze that let us scan and assess our surroundings. Without this integration, these movements would be erratic, out of sync, or entirely absent.
Coordinating the Senses of Balance and Space
While the superior colliculus manages the orchestration of head and eye movements, the vestibular nuclei within the brainstem maintain balance and spatial orientation. These nuclei receive input from the inner ear’s semicircular canals and otolith organs, which detect rotational and linear acceleration. From this information, the brainstem constructs a working model of the body’s position in space.
What makes the vestibular system so essential is that it doesn’t act alone. It continually interacts with visual and proprioceptive signals, comparing what the inner ear senses with what the eyes see and the skin feels. When these signals agree, balance is maintained with little effort. When they conflict—as in motion sickness or concussion—the result is nausea, disorientation, or postural instability.
The vestibular nuclei project to multiple regions, including the cerebellum, spinal cord, and ocular motor nuclei. These pathways ensure that visual focus is stable even when the body moves, and that posture adjusts automatically to changing conditions. Damage to these circuits, even subtle, can manifest as dizziness, blurred vision, or difficulty with coordination—symptoms often seen in patients recovering from mild traumatic brain injury.
Early Integration Enables Efficient Action
The brainstem’s role is not simply to receive multisensory input—it is to prepare the organism for timely, efficient responses. This capacity for action-oriented integration is especially crucial in unpredictable environments. A sudden stimulus—a rustle in the grass, a car horn—demands an orienting response. The brainstem enables this by linking sensory convergence with motor readiness.
This integration is largely pre-attentive. That is, it does not require focused attention or conscious awareness to operate. In fact, it functions best when automatic, allowing the cerebral cortex to remain free for higher-order planning and reasoning. This efficiency is not merely a convenience—it is a necessity for survival.
When the brainstem fails to integrate effectively, the entire sensorimotor system becomes noisy and uncertain. Movements become hesitant. Reactions are delayed. In such states, the burden of maintaining stability and coherence falls to the cortex, which can quickly become overwhelmed. What should be seamless becomes effortful. What should be automatic becomes laborious.
Developmental Implications of Multisensory Neuron Function
The capacity for multisensory integration does not emerge fully formed at birth—it is learned. In early development, neurons in the superior colliculus and other brainstem structures undergo a period of plasticity in which cross-modal experiences fine-tune their responses. An infant hears a parent’s voice and simultaneously sees their lips move; over time, the brain learns to align these signals into a single, reliable cue.
This developmental process is fragile. When disrupted—by premature birth, sensory deprivation, or neurological insult—it can compromise the brain’s ability to automatically coordinate sensory input. This may manifest later as difficulty reading, writing, or navigating complex sensory environments like classrooms or playgrounds.
Multisensory neurons, then, are not just passive conduits—they are shaped by experience. Therapies that provide controlled, repeated multisensory stimulation can help refine or even reestablish these integrations. This principle lies at the heart of interventions like OMST, which target the sensory foundation of function before attempting to address higher cognitive challenges.
Bottom-Up Processing: Why the Brainstem Matters First
Defining Bottom-Up and Top-Down Pathways
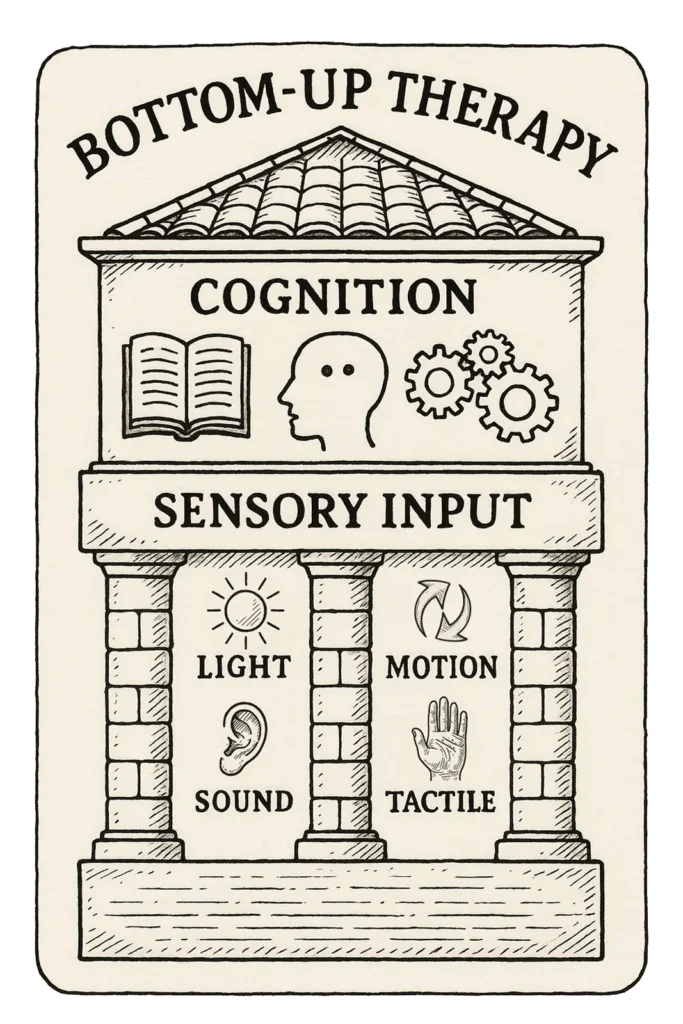
The human brain processes information in two primary directions: bottom-up and top-down. Bottom-up processing refers to the flow of raw sensory input from the body’s periphery to the brainstem and then to higher cortical centers. It is instinctive, fast, and foundational. In contrast, top-down processing begins in the cortex—shaped by memory, attention, and learning—and descends to influence perception and behavior.
The brainstem sits at the base of this flow, serving as the first true processor of incoming signals. It filters, integrates, and prioritizes sensory input before the cortex becomes involved. This filtering allows the brain to distinguish the rustle of wind from the snap of a twig, or to orient toward a sudden flash of light while walking. These are not conscious decisions; they are reflexive, governed by circuitry built to react before thought.
Top-down processing requires cognitive effort—planning a movement, solving a problem, interpreting language. But none of these functions can operate well unless the bottom-up systems beneath them are coherent and efficient. When foundational sensory input is disordered, the entire cognitive apparatus struggles to compensate.
The Subcortical Primacy of Early Learning
In development, bottom-up processing dominates the earliest stages of learning. Newborns do not reason or reflect—they feel, orient, and respond. Their brains are flooded with sensory information: sounds, sights, movement, touch. These sensations stimulate subcortical pathways that lay the groundwork for more complex skills.
The superior colliculus and vestibular nuclei begin aligning visual and vestibular signals in infancy, long before a child can speak or comprehend language. A baby’s first ability to track a parent’s face or turn toward a rattle emerges from these early integrations. Over time, repeated sensory experiences shape the neurons of the brainstem, fine-tuning their timing, sensitivity, and responsiveness.
This early period is critical. If disrupted—by injury, deprivation, or developmental disorder—the brainstem may not develop the reliable integration needed to support later learning. Children who struggle with attention, coordination, or sensory sensitivity often display signs of incomplete or inefficient bottom-up processing. Their difficulties are not rooted in willful behavior, but in the circuitry that forms the basis of attention and regulation.
Symptoms of Disordered Bottom-Up Integration
When bottom-up processing is impaired, the consequences ripple outward. A person may become overly sensitive to light, sound, or motion—or, conversely, under-responsive and sluggish. They may experience dizziness, confusion in crowded environments, or difficulty following verbal instructions when visual distractions are present.
These symptoms are especially common in post-concussion syndrome and certain neurodevelopmental conditions. Because the brainstem governs pre-attentive sensory modulation, damage or dysregulation in its circuits can make everyday environments feel overwhelming. A classroom becomes a minefield of competing signals. A supermarket triggers a flood of disjointed impressions. Even walking across a room requires deliberate effort.
Top-down strategies—like focusing harder, self-talking, or rehearsing routines—may offer temporary compensation. But they rarely solve the root problem. Until the brainstem’s foundational systems are re-integrated, the cortex must carry a burden it was never meant to bear alone.
Reclaiming Efficiency Through Bottom-Up Rehabilitation
Multisensory therapies like OMST are designed to reengage the brain’s bottom-up systems by stimulating them directly, without cognitive demands. By using light, motion, sound, and tactile input simultaneously, these interventions recreate the conditions under which multisensory integration originally developed.
This approach respects the primacy of subcortical processing. It does not ask the brain to “think its way out” of dysfunction. Instead, it provides structured sensory experiences that allow the brainstem to recalibrate—reducing sensory conflict, restoring automatic responses, and relieving the cortex from the work of constant compensation.
The clinical impact of this approach has been profound. Patients report improvements in balance, attention, speech fluency, emotional regulation, and general comfort in daily life. These gains are not the result of isolated skill training but emerge from a broader restoration of sensory coherence at the level of the brainstem.
When bottom-up processing is repaired, higher functions follow. Attention becomes more fluid, memory more accessible, mood more stable. This sequence is not just logical—it is biological. The brain cannot reach upward until it is steady at its base.
When Integration Fails: Brainstem Disruption and Dysfunction
The Cascading Effects of Brainstem Injury
When the brainstem is injured or functionally impaired, the consequences can be wide-reaching and insidious. Though small in mass, the brainstem anchors the nervous system’s sensory integration. Disruption here doesn’t just cause localized issues—it disturbs the timing, alignment, and regulation of information flowing to the cortex. This creates a bottleneck of disjointed perception and a compensatory overload on higher-order brain regions.
In cases of mild traumatic brain injury (mTBI), for instance, even when imaging shows no visible structural damage, patients may experience persistent symptoms: dizziness, blurred vision, light and sound sensitivity, nausea, and a pervasive sensation of being out of sync with the world. These are not imagined. They reflect real dysfunction in brainstem circuits responsible for fusing and filtering multisensory input.
Children with developmental delays often display similar symptoms. Difficulty concentrating, navigating spatial environments, or managing emotional reactions can stem from a brainstem that failed to adequately develop its automatic multisensory coherence. In both developmental and acquired cases, the resulting burden on the cortex leads to fatigue, irritability, and poor academic or social performance—not from lack of effort, but from systemic overload.
Sensory Fragility and the Breakdown of Autopilot
When multisensory integration breaks down at the brainstem level, what should be automatic becomes manual. The body is no longer able to regulate its reactions without cognitive effort. Activities that once required no thought—maintaining posture, walking in a crowd, processing conversation in a noisy room—now require constant, deliberate focus.
This phenomenon is often described by patients as “being stuck in first gear.” The brain cannot shift smoothly from input to response. The visual field may feel fragmented. Sound may be intrusive or disorienting. Motion may induce nausea or anxiety. These symptoms mimic or overlap with psychiatric disorders, but their root is neural disarray, not emotional imbalance.
Because of this fragility, traditional top-down therapies—talk-based counseling, cognitive training, even advanced academic instruction—may fail to take hold. The brain cannot absorb higher-level input when its base-level systems are unreliable. Until those systems are stabilized, every additional task feels like another layer of burden atop a structure too shaky to hold it.
Clinical Patterns and Diagnostic Blind Spots
Conventional assessments often overlook subcortical dysfunction. Standard neurological exams may appear normal, and imaging scans such as CT or MRI rarely detect deficits in brainstem integration. This has led to underdiagnosis or misattribution of symptoms in many patients—especially those suffering from post-concussion syndrome, long COVID neurological effects, or complex developmental delays.
Yet when clinicians look beyond structural markers and instead assess sensory processing, balance, pupillary reflexes, and visual motion sensitivity, patterns emerge. These patients are not unwell in abstract psychological terms—they are navigating a reality where the sensory world is fractured and unpredictable.
Research and case studies have shown that improvements in functional color fields, vestibular performance, and visual-evoked potentials often accompany symptom relief in patients undergoing therapies that directly target the brainstem’s sensory integration functions. These markers may provide more meaningful insight into recovery than traditional imaging alone.
Rebuilding the Foundation with Sensory-Based Interventions
Interventions that prioritize bottom-up recovery recognize that healing begins with coherence. They seek not to mask symptoms but to realign the nervous system by reintroducing structured multisensory input in a controlled, non-threatening environment. This is the philosophy behind Optometric Multisensory Training (OMST).
OMST incorporates light therapy, vestibular stimulation, auditory input, and somatosensory feedback in synchronized fashion. The therapy does not require the patient to analyze, verbalize, or problem-solve—it simply invites the nervous system to remember how to regulate itself. Over time, these repeated sessions retrain the brainstem to modulate incoming sensory streams and redistribute them in a harmonized way to higher regions of the brain.
Patients often describe the experience as subtle at first, but steadily transformative. Tasks that once felt taxing become fluid. Noise becomes tolerable. Reading comprehension improves. Movement feels grounded. These are not trivial gains—they mark a return of natural regulation, of the body’s autopilot quietly reactivating.
And from there, the rest of the brain can begin its work—not burdened by chaos, but built upon coherence.
Integration as Restoration
Returning to the Body’s Native Rhythms
Healing, when it happens at the level of multisensory integration, is not dramatic. It is quiet. A reduction in effort. A reclaiming of rhythms that once flowed unnoticed—how the eyes move in sync with the head, how the feet find balance without thought, how the senses gather the world and hand it gently to awareness.
Restoring function to the brainstem is not about maximizing performance. It is about normalizing perception. It is the difference between reacting and responding, between bracing against reality and moving through it with ease. For many, this restoration marks the first time in months or years that daily life feels manageable again. The fog lifts. The background noise recedes. The body becomes inhabitable.
What appears to be a miracle is often a reawakening of systems that were always there, waiting to be re-synchronized.
Preparing the Ground for Cognitive Growth
Just as a tree cannot grow in depleted soil, higher cognitive functions cannot flourish on a foundation of disordered sensory input. Reading, reasoning, speaking, and socializing all rely on the mind’s ability to ignore irrelevant stimuli, to prioritize what’s important, to stay grounded in space and time.
When the brainstem is healthy, it filters the world efficiently. It lets the cortex do its work. But when its signals are distorted or chaotic, every cognitive task becomes more difficult. Children fall behind not because they cannot learn, but because their brains are too busy trying to stabilize the input. Adults withdraw from life not from lack of will, but from neurological exhaustion.
By restoring multisensory integration, therapies like OMST do not replace education or counseling. They prepare the ground for those approaches to take hold. They give the brain its natural hierarchy back: sensation first, cognition second. And when that order is restored, learning becomes not only possible—but often joyful.
A Poetic Precision in the Brain’s Design
There is something quietly elegant about the way the brain works when it is well. The senses align. The body moves without friction. The mind follows, curious and clear. That this harmony begins in the depths of the brainstem—out of view, beneath awareness—is a reminder of how much of our humanity is shaped by processes we do not consciously direct.
The role of multisensory integration is not decorative. It is not supplemental. It is foundational. It is the scaffolding on which perception rests and the bridge across which experience flows. When it is fractured, life becomes unsteady. When it is restored, the world coheres again.
That restoration is possible—even after injury, even after delay—is not only a clinical truth. It is a human one. The brain does not forget its design. With the right inputs, even long-dormant systems can begin again. And in that beginning, not only function, but hope, returns.